"Mdm X walked into my clinic one day for her annual health screening with me. She is 49 years old and works as a corporate executive. She is well-groomed and has a strong scent of Chanel No. 5 as she walked in. Yet, below that strong perfume scent, there was an unmistakable smell of urine. It was something familiar to me from my days working in the hospital. As I went through her medical history and conducted a physical examination, I decided to ask her about her urinary symptoms. Suddenly, she broke down and started crying in my clinic…"
Does this situation strike a chord in you? Mdm X is suffering from what we call, urinary incontinence (UI). It is a treatable condition in which a person loses control of their bladder function. In Singapore, UI is more common than you think. However, it is said to be under-reported. Therefore, leading it to be under-diagnosed.
In this article, I will share with you everything you would need to know about urinary incontinence. I will go in-depth about the four different types of it as well as the causes and treatment options available for you.
4 main types of urinary incontinence
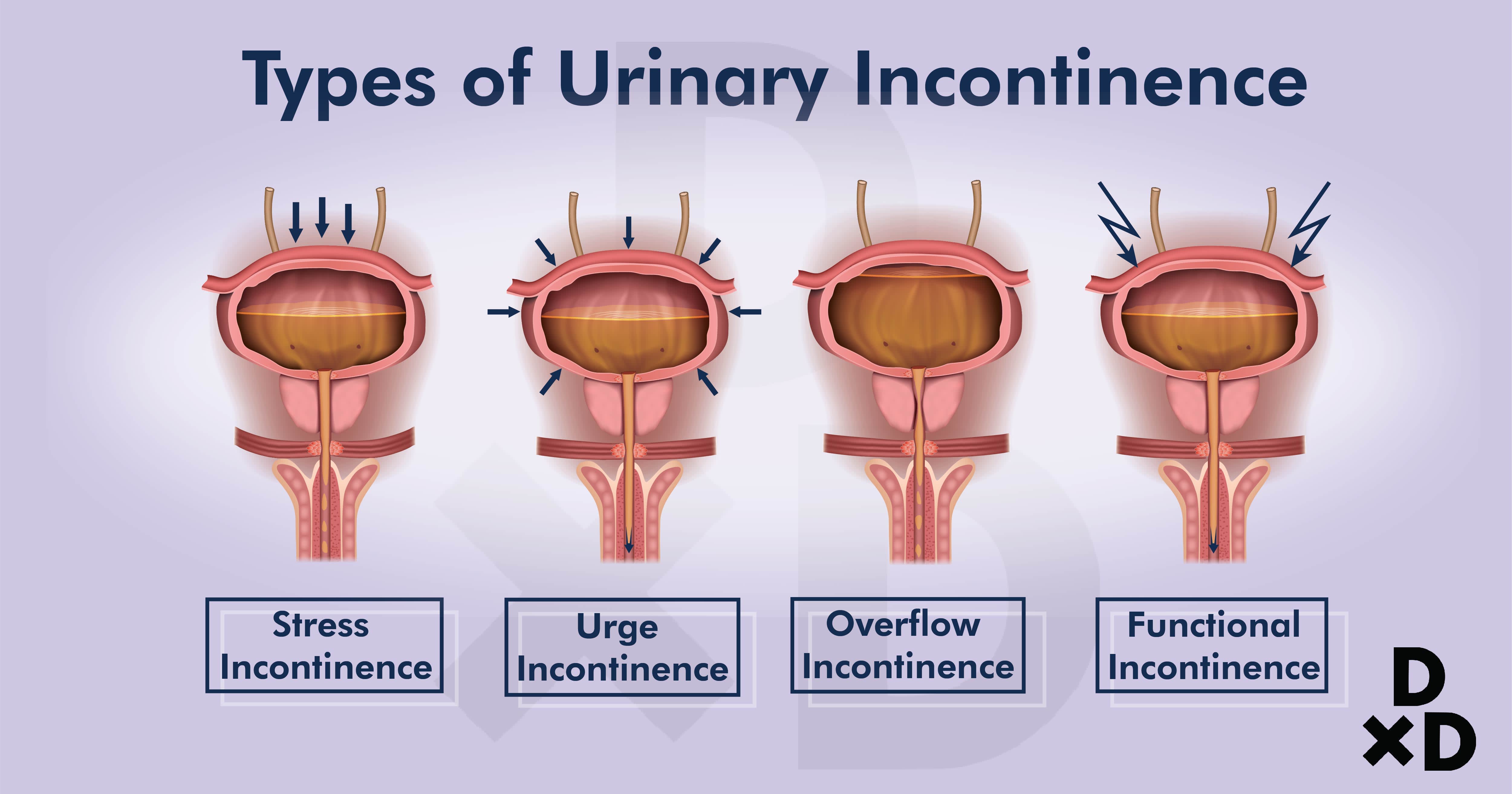
Urinary Incontinence happens when you cannot control your urine urges. Here are the four main types:
Types of Incontinence:
Causes:
Stress
Stress incontinence results when there is an increase in pressure within the abdomen. Urine may leak when sufferers:
- Sneeze
- Cough
- Laugh
Gym-goers may leak when they exert themselves. It happens when the muscles and connective tissues that control our flow of urine weaken.
Urge
Urinary incontinence results from bladder muscles that are hyperactive. It causes frequent urges to pass urine, even if the urine volume is low.
Those that suffer from UI may find themselves starting to leak before they manage to find a toilet. It can be from as little as a few drops to completely wetting themselves.
Often paired with:
- frequent urination and
- waking up in the middle of the night to pass urine.
Known as “Overactive Bladder Syndrome” in particular.
Overflow
Overflow incontinence results from:
- bladder muscles that are underactive or
- when urine outlet is blocked.
It causes the urine to remain in the bladder and leak out slowly.
Those that suffer from this type often feel that they have not emptied their bladders fully. During a visit to the toilet, urine may be dribbled out. Moreover, they may also experience leaking after.
Functional
People who have function incontinence do not have any problems with bladder storage or urinating. However, they are unable to empty urine promptly.
This could be due to physical problems such as arthritis or dementia [1].
Mixed
A combination of both symptoms of stress and urge incontinences.
Others
Other known causes are:
- Infection of the urinary tract
- Constipation
- High alcohol and caffeine intake
- Some medications
- Certain neurological conditions
- Some types of cancers
You may consult your doctor to know which type you are suffering from.
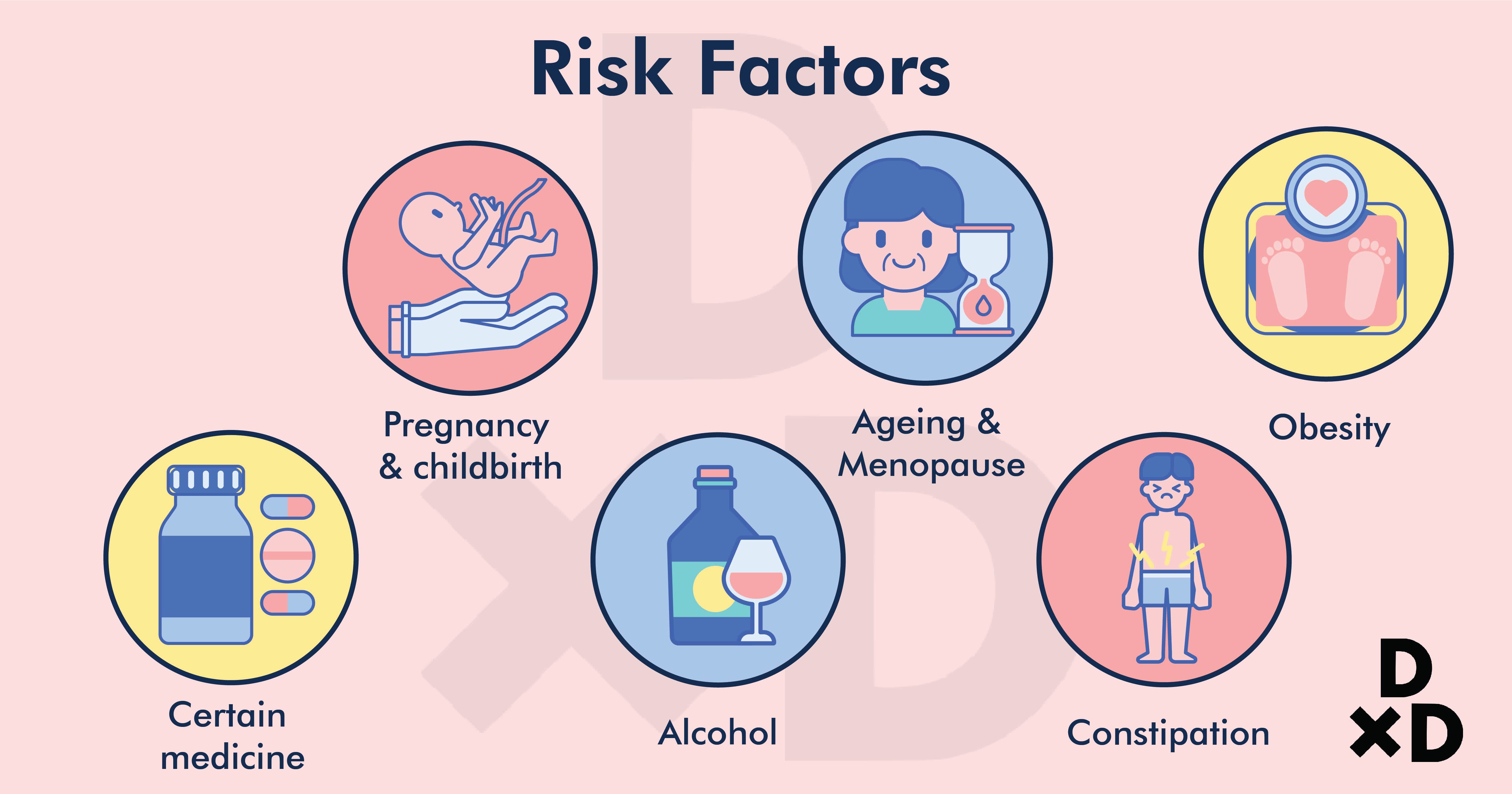
What are the risk factors of UI?
In fact, there are many risk factors for urinary incontinence. They are those that affect the muscles and tissues of the urinary tract. To list, it includes [2]:
- Pregnancy and Childbirth. This can stretch and weaken a woman's pelvic floor muscles.
- Ageing. As we age, our muscles and tissues of the urinary tract start to weaken.
- Menopause. The muscles and tissues of the female genital tract start to weaken during menopause.
- Obesity. The weight of being obese can add excessive stress to the muscles, thus, weakening them.
- Certain types of medications. There are a few types of medications out there that can cause or play a part in incontinence [3]
- Caffeine, alcohol and spicy food. These types of food can irritate the bladder. Hence, causing it to worsen incontinence.
- Constipation. It prevents urine to flow out as it normally should. Therefore, it may cause an Urge or Overflow incontinence.
How common is it?
Mdm X is just one out of the many patients who are affected. It affects about 30 to 40% of women worldwide. Of this group, less than half of them seek help for it [4].
In Singapore, the number of affected adults are estimated at 4.6% to 14.5%. These numbers are most likely to be higher due to the under-reporting of symptoms [5].
Patients usually avoid seeking treatment because of social embarrassment. They also have a misconception that this is part of our ageing process. Thus, this leads them to think that there is not much we can do about it.
Am I more prone?
In fact, urinary incontinence can affect anyone. It affects anyone of any age or gender. However, some groups can be more affected than others. Women and the elderly are likely to be more affected than men or children.
The most common causes in men are linked to both overflow and urge incontinence. Often, it is because of prostate issues like an enlarged prostate or after prostate surgery [3]. On the other hand, for children, it can be due to urinary tract infections or other congenital issues. Therefore, if you suspect that you might be suffering from UI, be sure to consult a doctor as soon as possible.
Also read: The Ultimate Guide to Prostate Cancer in Singapore (2021)
What is the diagnostic procedure like in Singapore?
Doctors can diagnose it in the clinic. The first step I would take would be to go through the history of my patient.
Targeted questions to find out the type of incontinence
- Does urine leak when you cough or sneeze?
- Do you feel repeated frequent urges to pass urine?
- Is there a mixture of both?
Possible contributing factors
- Pregnancy and childbirth history
- Menstrual history
- Past surgeries
- Chronic conditions like diabetes
- Long-term medications
- Symptoms of a urinary tract infection
- Dietary histories. How much caffeine and alcohol do they consume daily
- Amount of water drunk daily
- Bowel history
Social history
- How the symptoms have affected him/her socially
- Signs or symptoms of depression etc
Most of the time, the patient's history is enough for me to diagnose urinary incontinence. I will still proceed to find out if there are any other contributing causes. For example, the presence of masses in the abdomen or an enlarged fibroid or prostate.
I will also perform a simple urine dipstick. This is to rule out any urinary tract infections.
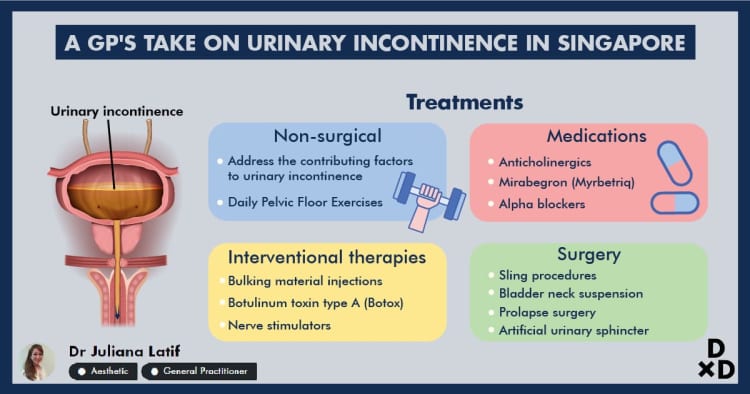
How is urinary incontinence treated?

"In between sobs, Mdm X shared with me that she has been having symptoms of urinary incontinence for the past year. She frequently feels the urge to pass urine and leaks urine whenever she laughs or coughs. It seems to be getting progressively worse, up to the point where it has started to affect her work life and personal relationship with her husband. She feels that her colleagues have been avoiding her and she has also started to be more withdrawn from them. Her husband has also been complaining of a urine stench whenever she is around him. She feels like nothing can be done about this as this is part of her ageing and menopause process…"
I reassured her that that is not true. In fact, you can do something about it. Urinary incontinence is not a natural process of ageing! Do not accept the status quo. There are many treatment options available. Besides that, some of which does not require you to go through surgery.
Non-surgical
You may start to cut down on the factors that may be contributing to urinary incontinence. For example:
- For patients who are obese, they can start an exercise regime to lose weight
- Caffeine, alcohol and spicy food can be cut down from your diet.
In addition, be sure that you are taking in enough fibre. This reduces the chances of constipation
Daily Pelvic Floor Exercises
Kegel exercises help to strengthen the pelvic floor muscles. These muscles are in charge of supporting the uterus, bladder, small intestines and rectum [6].
- Start by identifying the correct pelvic floor muscles. The best way to do this is to try and stop your urine halfway through urinating. The muscles activated to do that are your pelvic floor muscles.
- After identifying, you may then practise Kegel exercises. For beginners, you may lie down on the floor. Afterwards, start to tighten and relax your pelvic muscles for three seconds each. Repeat these 15 times.
- It is crucial to do Kegel Exercises daily in sets of three. This will help to strengthen your pelvic floor muscles. Thus, reducing the incidences of stress incontinence. Your incontinence should start to improve after three to six weeks.
- An important note is to focus on tightening only your pelvic floor muscles. You may find it hard to coordinate their muscle movements at first. However, you could end up tightening your abdominal muscles instead. In some cases, you may leak during Kegel exercises. Despite that, do not give up! You should continue to keep trying! [7].
Medications
Anticholinergics
It is used to treat urge incontinence. In particular, it can calm an overactive bladder. Here are some examples of this type of medication: oxybutynin (Ditropan XL), tolterodine (Detrol), darifenacin (Enablex) [8].
Mirabegron (Myrbetriq)
Similarly, it helps to treat incontinence. It helps to relax the bladder muscle and increases the amount of urine your bladder can hold.
Alpha-blockers
In men with urge or overflow incontinence, these medications relax the bladder neck muscles as well as the muscle fibres in the prostate. In addition, the bladder can empty much easily when these muscles are relaxed. Here are some examples: tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo) [8].
Interventional therapies
Bulking material injections
Synthetic material is injected into the tissue that is surrounding the urethra. Hence, helping to keep the urethra closed and reduce leakage. This procedure needs to be repeated regularly as it is not as effective as other treatments.
Botulinum toxin type A (Botox)
Injecting Botox into the bladder muscle may benefit those who have an overactive bladder. However, it is normally prescribed to people only if the first-line options have not been successful.
Nerve stimulators
A device will be implanted under your skin near your buttock. It will deliver painless electrical pulses to the nerves involved with bladder control (sacral nerves). Stimulating these sacral nerves controls urge incontinence if other therapies have not worked. The device will be connected to wires on the lower back, above the pubic area or, with the use of a special device, inserted into the vagina [8].
Surgery
For severe cases of UI which do not respond to the above therapies, surgery might be an option. Like with any surgery, these surgery comes with risks. Therefore, you should talk with your urologist to understand the possible risks and benefits of the surgery. Below are the different types of surgery that you may undergo.
Sling procedures
Strips of your body's tissue, synthetic material or mesh are used to create a pelvic sling. It is positioned around your urethra and the area of thickened muscle where the bladder connects to the urethra (bladder neck). The sling helps keep the urethra closed, especially when you cough or sneeze. It is used to treat stress incontinence.
The most common type in use is tension-free vaginal tape (TVT). Other versions of the slings include TVT-O, TVT-exact and TVT-abbrevo [9].
Bladder neck suspension
This procedure is designed to give support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision. It's done during general or spinal anaesthesia.
Prolapse surgery
For women with mixed incontinence and pelvic organ prolapse, surgery may include a combination of both sling procedure and prolapse surgery.
Artificial urinary sphincter
In men, a small, fluid-filled ring is implanted around the bladder neck. This keeps the urinary sphincter shut until you're ready to urinate. To urinate, you press on a valve implanted under your skin that causes the ring to deflate. Hence, allowing urine to flow from your bladder.
If you unsure which is more suitable for you, be sure to discuss the risks and benefits with your doctor.
Conclusion
"Mdm X found that her symptoms have coincided with the onset of her menopause. After starting on Kegel exercises as well as two treatments with the incontinence laser, she came back two months later with all her symptoms resolved. She is much happier and feels more refreshed and energetic to cope with the challenges at work."
In short, urinary incontinence is a common problem. However, it should not be part of your natural ageing process. Many treatment options are available to reduce or even treat it. The key is to speak with your doctor about it and work with him or her to find an option that works best for you.
%treatmentquote title=Get quote for Urinary Incontinence%
Dr Juliana Latif is a family physician and Aesthetic Medicine doctor with Fusion Medical. In addition, she graduated with an MBBS from King’s College London and also obtained a GDFM from the National University of Singapore. Moreover, she is a member of the Singapore Medical Council.
Read more of Dr Juliana Latif's QnA here.
References
1. Harvard Health Publishing. Types of urinary incontinence - Harvard Health. Harvard Health.
2. Urinary incontinence - Symptoms and causes. Mayo Clinic.
3. Harvard Health Publishing. Medications that can cause urinary incontinence - Harvard Health. Harvard Health.
4. Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F. Risk factors for urinary incontinence among middle-aged women. American Journal of Obstetrics and Gynecology. 2006;194(2):339-345.
5. How C, Quah J. Managing urinary incontinence in the community. Singapore Medical Journal. 2013;54(8):420-424.
6. Urinary Incontinence in Older Adults. National Institute on Aging.
7. National Institute of Diabetes and Digestive and Kidney Diseases. Kegel Exercises | NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases.
8. Urinary incontinence - Diagnosis and treatment - Mayo Clinic. Mayoclinic.org.
9. SingHealth - Urinary Incontinence. Singhealth.com.sg