Sleep apnea is a condition in which the upper airway is either too narrow, because of tissue swelling or anatomical obstruction, or too floppy. This results in the sufferer receiving a disrupted supply of oxygen, which then often leads to a night of poor disturbed sleep.
As an ear, nose and throat (ENT) specialist with key interests in paediatric ENT, I have come across many cases of sleep apnea in children.
Paediatric sleep apnea has wide-ranging effects if it’s left untreated or not treated properly. However, its symptoms and long-term effects on children's growth are not well-understood by parents.
In this article, I explain how untreated sleep apnea can affect your child's well-being and growth, and what the available treatments for sleep apnea are.
What is paediatric sleep apnea?
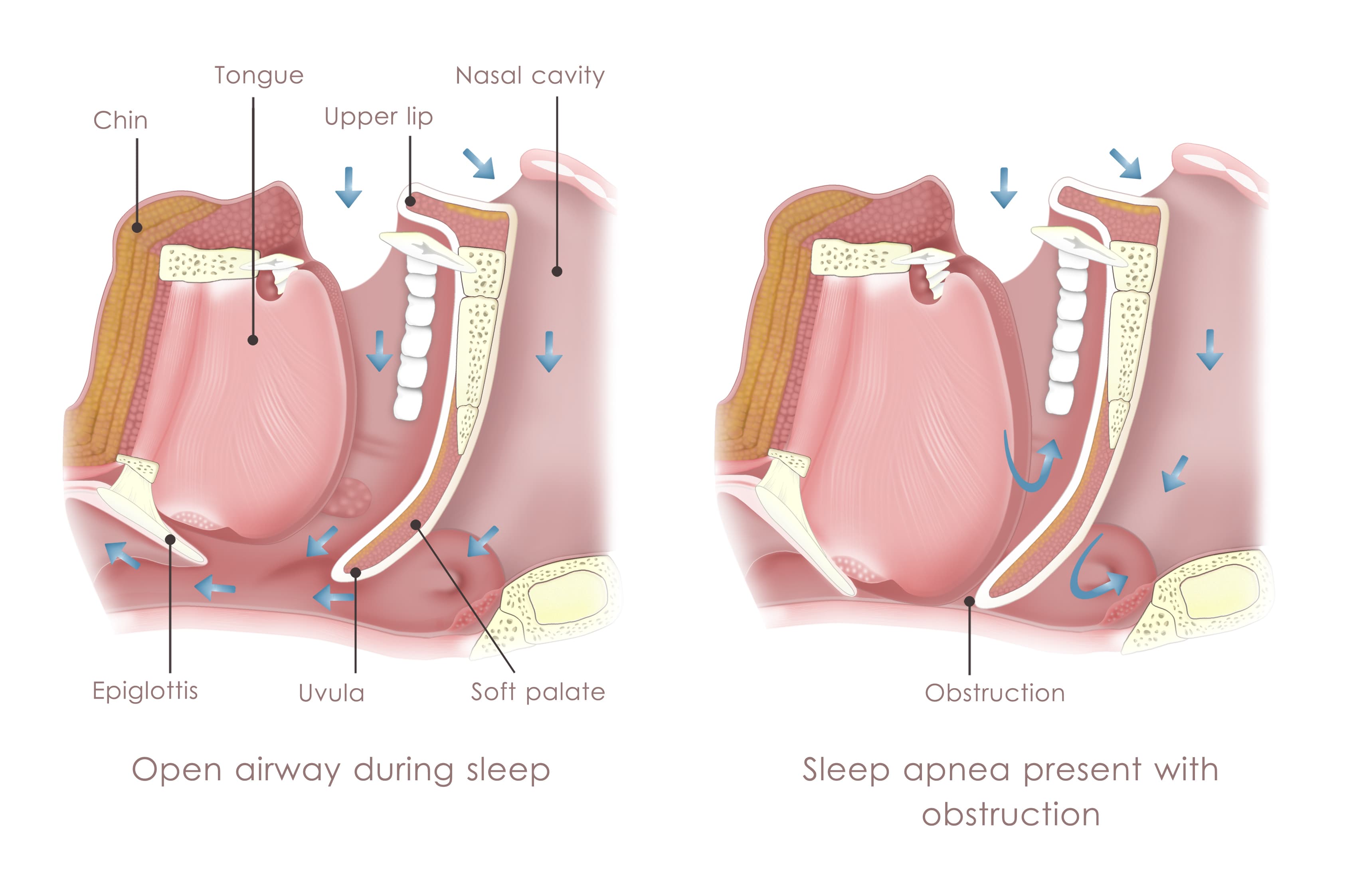
Paediatric sleep apnea simply refers to sleep apnea that occurs in children. As previously mentioned, sleep apnea is when the upper airway is too narrow or too floppy [1]. When the child has a very small airway, it can collapse or become obstructed. This results in the child receiving a disrupted supply of oxygen, which then often leads to a night of poor, disrupted sleep [2].
Paediatric sleep apnea has wide-ranging effects if it’s left untreated or not treated properly [2].
Parents are often unaware their child has sleep apnea
I find that it is quite under-diagnosed in our community. Unlike in adult sleep apnea, where patients can articulate that they are tired or have unrefreshed sleep, in children, this condition could be the reason for [3]:
- bedwetting
- poor growth/weight gain
- crankiness or hyperactivity
- poor school performance
- behavioural or concentration issues
The difference between snoring and sleep apnea in children
Snoring is when the airway vibrates as a result of some narrowing. It signifies that there is some obstruction in the airway [4]. A child can snore without having sleep apnea, but any child that snores regularly really needs to be assessed for sleep apnea [5].
Sleep apnea, on the other hand, normally presents with snoring and disturbed restless sleep [6]. However, in some cases, the child may not even snore that much because his/her airway keeps getting blocked, resulting in breathing pauses or choking. The child might sleep with his/her head facing upwards and mouth open as this position opens the airway (very similar to the chin lift and jaw thrust that we use in cardiopulmonary resuscitation).
A small or obstructed airway may result in an unusual sleep posture e.g. a frog-like position, or cause other symptoms like mouth breathing, snorting, frequently waking up at night, night terrors and bedwetting.
I find that it is sometimes not easy for parents to recognise that their child has sleep apnea as the signs and symptoms may not be obvious.
How paediatric sleep apnea affects your child’s sleep

In essence, to have a good night’s sleep, you will want to make sure that the upper airway is clear [7]. In children, it is most frequently their adenoids, tonsils and nose that cause narrowing or obstruction [8].
Of course, some children with congenitally small jaws, or those with Down syndrome, facial abnormalities and neurological conditions, also have an increased risk of getting sleep apnea [9].
When the airway is obstructed, the oxygen levels often start to drop and this will result in the body being stressed [10]. Unfortunately, it is when children are in deep sleep or dream sleep that their airways are the most floppy, and the drop in oxygen will then trigger the brain to wake them up or change their sleep position.
Lowered oxygen levels can also result in heart problems, as the heart has to work harder when the oxygen level drops [11]. In fact, as early as the 1960s, there were reports of children with heart failure who had the condition reversed just by removing their adenoids [12]. Even up to now, there are case reports of children who develop heart failure as a result of large adenoids [8].
I find that parents with children who have sleep apnea often do not sleep well themselves, since their sleep is often disrupted by their child waking frequently or having behavioural issues.
How paediatric sleep apnea affects your child’s growth
Growth hormone is secreted during deep sleep [13]. As long as your child’s airway is obstructed, it will result in much lighter sleep and less secretion of growth hormone.
Children who require growth hormone replacement are now increasingly referred for sleep studies first before starting growth hormone replacements. Children with poor growth or poor weight gain are also frequently referred for sleep studies [14].
In my experience, it is not uncommon to see children grow better after their airways are cleared and their sleep quality improves.
The other issue is facial growth impairment in some of these children [15]. There is now increasing data that children who breathe through their mouths end up with narrowed jaws and sometimes longer faces. The narrowed jaws then predispose them to smaller airways as adults [16].
Identifying the signs and symptoms of sleep apnea in children
Common symptoms at night:
- Disturbed restless sleep
- Laboured breathing
- Sweating
- Frequent snoring
- Night terrors
- Choking while sleeping
- Bedwetting
- Frequently sleeping with an open mouth
- Unusual sleeping positions (e.g. frog-like posture, tilted chin): these unusual sleeping positions are the body’s natural attempts at opening up the airway
Common symptoms during the day:
- Behavioural, concentration issues
- Unrefreshed sleep, daytime tiredness
- Hyperactivity issues
- Attention issues
- Poor school performance
Many studies have shown that sleep apnea affects neurocognitive performance, so children with sleep apnea may not do as well in school as compared with kids who breathe properly and have good sleep quality.
Other signs and symptoms
- Chronic mouth breathing posture
- Swollen nasal tissue
- Swollen tonsils and adenoids
- Small chin
- Failure to thrive
- Poor growth
- Cardiovascular issues, including blood pressure issues [17]
What are some risk factors of paediatric sleep apnea?
Children with certain congenital issues are more likely to get sleep apnea [18]. For example, if your child is born with a very small jaw, his/her airways are pushed backwards.
Also, children born with Down syndrome have larger tongues that can obstruct airways [19].
Other risk factors include the patient having [20]:
- enlarged tonsils and adenoids
- Achondroplasia (short-limbed dwarfism)
- Facial abnormalities
- Neurological conditions like cerebral palsy, etc.
Which doctor do I visit if my child has paediatric sleep apnea?
You should certainly see a doctor who specialises in sleep apnea and is comfortable with children. This ENT doctor will determine where the levels of obstruction are with an endoscope, and frequently start treatment with medication.
A dedicated paediatric sleep physician is normally a respiratory doctor who has special training in performing sleep studies in kids.
Why is mouth breathing in children a problem?

When babies are first born, they are obligate nose breathers, meaning that they can only breathe through their nose. It's only after 6 weeks that we learn to mouth breathe [21].
The need to open our mouths to breathe frequently signifies a blockage in the airway. So, constant mouth opening or the constant posturing of our neck forward are signs of a blocked airway.
If your child is a chronic mouth breather, it can affect the way the face and jaw grow. He/she is more likely to end up with a narrowed jaw and face, which can often result in teeth crowding.
As our jaws are 60% grown by age 4 and 90% grown by age 12, it is important to fix this problem early.
What happens if paediatric sleep apnea is not treated?

When paediatric sleep apnea is not treated, your child is more likely to [22]:
- perform poorly in school due to impaired sleep quality
- have behavioural, concentration, attention issues
- have growth issues sometimes
- have cardiovascular/blood pressure issues occasionally
Sleep apnea treatment in Singapore
When treating paediatric sleep apnea, we look at the patient's symptoms and the results of a sleep study.
Allergen avoidance
In mild cases, we always start with conservative means, such as educating the patient on avoiding allergens in the environment and food, and treating allergies. I normally prescribe nasal steroids and nasal normal saline douches as well, to rinse their noses.
Sometimes we prescribe antihistamines or other allergy medication to treat the allergies involved [23]. If the child is obese, we would ask him/her to lose weight.
Childhood Adenotonsillectomy Trial (CHAT)
For obvious sleep apnea, in which the child stops breathing more than 5 times an hour, the recently concluded Childhood Adenotonsillectomy Trial (CHAT) showed that removing adenoids and tonsils improved symptoms, quality of life and behaviour [24].
I normally treat the nose as well as the front part of the nose (or nasal valve area) as it is the site of most resistance in our upper airway. In a few selected cases, we would sometimes do surgery on the palate, tongue or tongue tonsils if we find that there is narrowing or obstruction in that area.
Palate expanders
In selected cases, the other form of treatment that I sometimes find helpful is the use of palate expanders to expand the palate. This is important because the width of the upper palate determines the lateral size of the airway. We work with dentists who put these expanders on for children when they are mature enough to accept them [25].
Myofunctional therapy
Myofunctional therapy has also been advocated overseas for the treatment of sleep apnea. These exercises increase the muscle strength of the upper airway. Most of this data is however derived from the adult apnea population [26].
Treating persistent sleep apnea with CPAP

In cases where the child has persistent sleep apnea despite the above treatments, then we will also consider using assisted ventilation such as a Continuous Positive Airway Pressure machine (CPAP).
Treatment with the CPAP machine is suitable for both children and adults with sleep apnea [27]. We use it sometimes if there is residual sleep apnea post-surgery or if the parents do not want surgery.
Other treatments
Tracheostomy has very occasionally been used for patients with very severe apnoea associated with heart issues etc., especially if there are congenital facial deformities [28].
Costs of treating paediatric sleep apnea
The pricing is in a wide range as it depends on what needs to be done. We follow the Ministry of Health (MOH) pricing guidelines. An inpatient sleep study will normally cost between $2,000 and S3,000 in the private sector.
Can I claim MediSave for treatment of paediatric sleep apnea?
Yes, it is claimable. But it doesn’t cover the whole cost of private-sector treatment.
Depending on the class you choose, it may or may not cover the whole cost of public-sector treatment.
Conclusion
Being able to breathe well is essential to sleeping well and ultimately to living well. Parents may not realise it, but if your child is struggling to breathe, it often affects them in many ways – sleep quality, ability to concentrate, risks of behavioural issues, performance issues as well as other physical sequelae that affects growth and the cardiovascular system.
Treating paediatric sleep apnea is important and provides not only immediate but also long-term benefits to your child’s quality of life.
Dr Adrian Saurajen is an ear, nose, and throat surgeon at Gleneagles Hospital, Singapore. He sub-specialises in sleep medicine and surgery. Outside of his clinical practice, Dr Saurajen is actively involved in research, forums, and conferences. He graduated from the University of Sydney, and worked at the Royal North Shore Hospital in Australia before coming back to Singapore.
