Introduction
Osteoarthritis is a painful condition that’s due to wear and tear in your joints as you grow older.
The supportive tissue in your knee joint acts like the suspension system in a car, absorbing all the shocks from the physical activities in your daily life, such as:
- walking
- running
- climbing the stairs
- jumping
Now imagine what will happen to the suspension after the same car has been driven for over 60 years!
It’s no wonder that half of the people over 65 years old have osteoarthritis [1], which makes up around 31 million adults in the U.S. in 2018 [2].
While osteoarthritis is not reversible, it’s possible to slow its progress and reduce the amount of pain you feel. Read on to find out more!
What causes osteoarthritis?
To understand how osteoarthritis occurs, you need to understand how your joints work. Your joints are surrounded by something called a joint capsule. This joint capsule has a layer of the film around it called the synovial membrane.
This membrane secretes synovial fluid between your bones, which lubricates the area to facilitate movement and nourishes the cartilage that cushions your joints. The cartilage is important as it allows for complex movement.
As osteoarthritis grows worse, your cartilage wears out, deforming the bone structure and causes inflammation which thickens the synovial membrane that wraps around the capsule.
This thickened synovial membrane produces/secretes excessive fluids with unwanted inflammation promoters that further damages tissues in the joint capsule, including the cartilage.
What are the symptoms of osteoarthritis?
Osteoarthritis can affect any joint in your body, including your:
- Knees
- Hips
- Spine
- Hands
Common symptoms of osteoarthritis include:
- Stiffness, where you find it harder to move the affected joint.
- Tenderness, the discomfort you feel when you press down on the affected joint.
- Joint aches and pain, especially when you move it.
How do doctors diagnose osteoarthritis in the U.S.?
Osteoarthritis occurs slowly, over time. In the early stages, you might only be able to feel pain only when stressing the affected joint, such as running. Taking your medical history and a complete physical examination is the first step to detecting problems.
If there are issues that warrant further investigation, such as persistent pain, then your doctor will ask for an X-ray to rule out other causes of pain and examine bone damage. You might need an MRI (Magnetic Resonance Imaging) to check the cartilage [3] [4].
The doctor might also ask for an Arthroscopy, where an instrument is used to visualize the joint interior. Finally, you might require a ‘joint aspiration’, where fluid is taken from the affected joint and examined for clues on the kind of arthritis you have.
In the U.S., the southern states have the highest percentages of doctor-diagnosed arthritis [34] including osteoarthritis, notably:
- Alabama
- Tennessee
- Virginia
- West Virginia
How does osteoarthritis differ from rheumatoid arthritis?
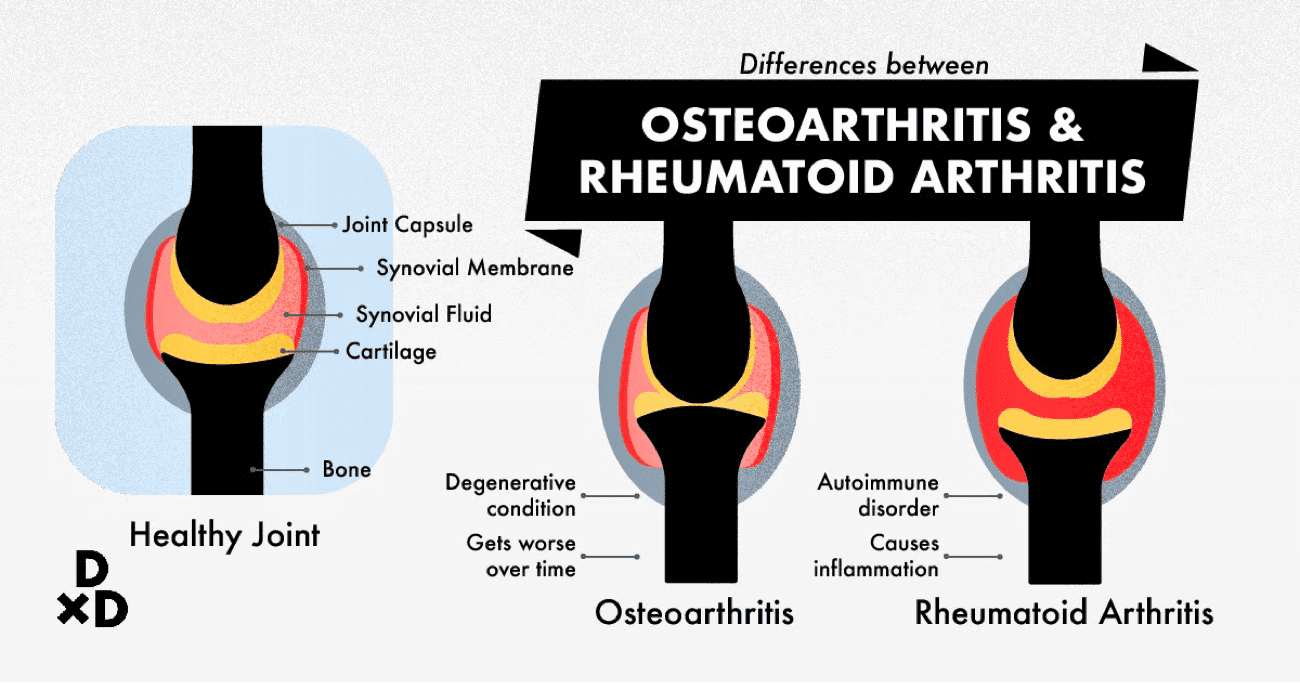
Similar to osteoarthritis, rheumatoid arthritis can also lead to inflammation, stiffness and pain of your joints.
However, the cause of inflammation is different. Rheumatoid arthritis is a form of autoimmune disorder, meaning your body mistakenly treats the joint capsule and its tissues as foreign matter and attacks them, causing the inflammation [5].
Osteoarthritis was once considered a non-inflammatory syndrome, with the cartilage being worn down over time. However, recent research shows that there is also an inflammatory process implicated in osteoarthritis [6].
Both forms of arthritis are very difficult to treat and often have no cure [7], although you can manage the symptoms and pain levels.
Does Medicare cover your osteoarthritis treatment in the U.S.?
Only some Osteoarthritis treatments are covered by Medicare, namely parts A, B, and D [32] [33].
- Medicare part A covers inpatient hospital and surgical care.
- Medicare part B covers the necessary diagnostic tests and surgical fees. Part B also covers physical therapy, paying up to 80% of charges.
- Medicare Part D covers most prescription drugs, but the specific medical formulary differs between plans. Over-the-Counter (OTC) drugs are usually not covered by Medicare.
What roles do exercise and physiotherapy play in your osteoarthritis treatment?
Being overweight and obese increases the strain on your joints, especially your knee joints. It can also lead to low-grade inflammation. By strengthening your muscles, increasing flexibility, and reducing fat in your body, you reduce the strain your joints need to bear. In most cases, tailored exercise helps in improving function and reduces pain [8].
There is a wide range of physiotherapy treatments available, ranging from massage to Pulsed Radio-Frequency treatment. These therapies can help with the perception of pain, particularly early on or after surgery, and do not have many negative side effects besides potential discomfort [9].
There is also occupational physiotherapy, where an occupational physiotherapist works with you to adapt your living and working space to reduce the pain you feel. For example, you might be encouraged to install a non-slip chair in your shower area if you have knee osteoarthritis.
How can you manage osteoarthritis and improve your quality of life?
The Centers for Disease Control and Prevention (CDC) recommends the following self-management strategies [31].
Join a self-management class: The CDC can point you to recommended self-management education programs to learn how arthritis affects you and assists you in treating symptoms.
Get physically active, but protect your joints: Take steps to eventually reach the 150 minutes of exercise recommended per week. This doesn't necessarily mean rigorous exercise where you sweat and exert yourself; moderate exercise like brisk walking at 3-4mph counts!
Make sure to avoid high impact sports like running.
You can join an activity program to learn how to exercise safely and in a communal setting. This is closely related to the next recommendation.
Lose weight: Getting physically active means that you will be putting pressure on your joints. Losing weight will help reduce this pressure and improve bone function.
Follow your recommended treatment plan: Keep close communication with your doctor as you learn what to do and follow the treatment plan religiously.
Common osteoarthritis treatments in the U.S.

Cost of Traditional Treatments for Osteoarthritis in the U.S.
The treatments in the table below are arranged in the order which people normally take them.
First, you might try out Tylenol to see if it has any pain-relieving effects. If not, osteoarthritis sufferers typically move on to a stronger painkiller in the form of either NSAIDs or COX-2 Inhibitors.
If that doesn't help, your doctor may decide to give you intra-articular Injections. Lastly, if all else fails, your doctor may recommend that you get a knee replacement - a fairly major surgery that will put you out for 6 months to a year!
Treatment
When to get treatment and when to avoid
Cost (USD)
Tylenol (paracetamol or acetaminophen)
First-line treatment
$15 per 50 tablets
NSAID
Second-line treatment. Do not take if you have irritable bowel syndrome or have had gastrointestinal problems
$5-$70+ per 90 tablets depending on the type of NSAID. Some tablets can cost more than $200
Intra-Articular Injection
Last line of treatment before surgery. Do not take if you have hypersensitivity to steroids, or there is severe skin/bone degradation.
Corticosteroids: $98-$110 per shot
Hyaluronic Acid: $310 per shot
Joint Replacement
Surgical option. Do not go for surgery if you have knee sepsis or peripheral arterial disease.
$50,000 to $70,000, depending on extra charges made.
Tylenol
Tylenol is also known as Acetaminophen or Paracetamol [10] [11]. It's a drug that is easily available for fever and pain relief. If your condition is mild to moderately severe, you can try Tylenol as a first-line medication.
While it is not as toxic as some of the treatments detailed below, it’s easy to forget that just because Tylenol is common does not mean it is ‘totally safe’.
In fact, Tylenol can lead to high levels of aminotransferase, which can result in liver damage. Research is also mixed about how effective it is for osteoarthritic pain.
NSAIDs (NonSteroidal Anti-Inflammatory Drugs)
NSAIDs include medications like aspirin, ibuprofen, and celecoxib [12].
These drugs work by blocking the production of cyclooxygenase enzymes, also known as COX-1 and COX-2.
As a result, these enzymes help to create a group of compounds called prostaglandins that result in inflammation. By blocking COX-1 and COX-2, NSAIDs help to reduce inflammation, which slows the progress of osteoarthritis.
However, unwanted side effects of NSAIDs include stomach pain, stomach ulcers, and headaches. There may also be unwanted interactions with other medications.
COX-2 (Cyclooxygenase-2) inhibitors
COX-2 inhibitors [13] are a specific type of NSAID, such as Etoricoxib and Celecoxib.
COX-2 inhibitors affect only COX-2 enzymes. As such, there are decreased incidences of gastric discomfort, gastric ulcers, and other upper gastrointestinal problems.
However, COX-2 inhibitors result in an increased risk of hypertension, heart failure, oedema, and other cardiovascular diseases.
The only COX-2 inhibitor available in the U.S. is Celecoxib, brand name Celebrex.
Intra-articular injections for Osteoarthritis
More non-surgical options include injections with hyaluronic acid, corticosteroids, or platelet-rich plasma [14]. These injections are the last resort before surgery. They work in different ways, depending on what kind of injection you receive.
Injections typically serve only as short-term solutions. This means that you’ll have to go back for injections periodically to maintain the effects.
Types of Intra-articular injections for Osteoarthritis
Corticosteroids
One of the first substances used for this kind of injection. Corticosteroids slow your immune system down, which results in less inflammation.
The research on corticosteroids for osteoarthritis is mixed, leaning towards more disappointing results. That does not mean it will definitely not work on you, but you must be prepared for a possible lack of significant results [15].
Hyaluronic Acid
Hyaluronic Acid is important and required for the body to create synovial fluid, which lubricates your joints. Hyaluronic Acid injections are among the safest injection choice. However, it might take up to 5 weeks for you to fully benefit from the treatment [16].
Platelet-rich plasma
I discuss this treatment option under ‘new, recent treatments for osteoarthritis’.
Joint Replacements for Osteoarthritis
As a last resort for treatment of serious osteoarthritis, you can opt to have a joint replacement. In a joint replacement, a scan of the affected joint structure is taken. With the information, a replacement joint, made of several metals and plastic, is prepared.
Then, under general anaesthesia, the surgeon removes the worn-out cartilage and the joint is cemented on the bone.
While you may be immobile for the first day of recovery, you will need to move and go through physical therapy to move the joint properly [17].
New, recent treatments and other alternatives for osteoarthritis in the U.S.

Cost of Osteoarthritis Treatments and Alternatives in the U.S.
Most of these treatments are still new and being tested, with research being mixed on whether they work or not. Usually, more time will be needed to confirm or disprove their effectiveness over time [18]. They range from supplements to medical procedures that have been used in other conditions.
Treatment
Cost (USD)
Japanese White Turmeric
$38-$45 per bottle, depending on whether or not you buy in bulk
Mesenchymal Stem Cell Therapy (MSCs)
$3,000-$5,000 per knee
Platelet-rich plasma injections
$350 per shot
Botox (Botulinum toxin) injections
$125-$500 per shot
Cooled Radio Frequency Ablation (C-RFA)
$5,000-$7,000 per knee
Also read: The Ultimate Guide to Supplements for Joint Health in Singapore (2021)
Supplements for Osteoarthritis—Japanese White Turmeric
Japanese White Turmeric [19] contains a compound called Labdane-type Diterpenes, which has anti-inflammatory properties that can lead to reduced pain. It’s also clinically proven to slow down the progression of osteoarthritis.
Till date, there are no known adverse side effects and no known interactions with other drugs. Beneficial effects take place about 2-3 weeks after starting on it. However, as with other supplements, talk to your doctor about taking it simultaneously with other medications or when you are pregnant.
Mesenchymal Stem Cell Therapy (MSCs)
MSCs [20] come in the form of an injection. See more about intraarticular injections below. MSCs are cells found in the bone marrow that can develop into many different types of cells, like fat or bone cells.
Researchers have managed to develop these cells such that they can develop into beneficial cells that repair joint tissues, counteracting inflammation. Research on this treatment is still in its early phases, but so far results have been promising, with pain reduction lasting for at least 6 months.
One type of MSC being studied is Bone Marrow Aspirate Concentrate (BMAC). One study finds injecting BMAC to be safe and could provide long-term benefits without complications [21]. The American College of Rheumatology does not recommend stem cell injections for knee/hip osteoarthritis, according to a 2019 update [30].
Platelet-rich plasma injections
Plasma refers to the liquid carrying your red blood cells, while platelets are blood cells that encourage blood clotting and healing functions. This treatment uses your own platelets to encourage tissue healing around the affected joint.
As one of the newer intraarticular injection treatments, more research needs to be done to ascertain the safety and efficacy of this treatment [22] [23]. However, the American College of Rheumatology does not recommend platelet-rich plasma injections for knee/hip osteoarthritis, according to a 2019 update [30].
Botox (Botulinum toxin) injections
You may know of Botox through aesthetic treatments. Botox works by paralysing the surrounding muscles. Research is slow on applying Botox to osteoarthritis, with current studies in conflict with one another. You may have to go for repeat injections to see an effect [24].
Botox injections are currently not recommended for knee/hip osteoarthritis, since there are fewer studies available [30].
Cooled Radio Frequency Ablation (C-RFA)
C-RFA uses magnetic fields and electricity to generate heat, which surgically destroys certain nerves and tissue around the joint. With the nerves unable to function, you will feel less pain in the surrounding area. As the treatment is very precise, you do not have to worry about losing sensation in areas other than around the joint.
The success of this treatment depends on how your body is shaped and whether the doctor can locate and reach the appropriate nerves. You must also keep in mind that the long term effects of C-RFA are unknown as pain relief was only tracked for 6 months [25].
Radiofrequency ablation is conditionally recommended for patients with knee osteoarthritis [30].
***********This educational article was brought to you by Tumeron Joint.***********
More on Japanese White Turmeric for osteoarthritis
It is worth trying Japanese White Turmeric as your first option since it does not have any side effects associated with it compared to all the other options available. In particular, Japanese White Turmeric is a supplement for osteoarthritis.
Japanese White Turmeric is a type of turmeric currently only grown in Kyushu, Japan. Unlike other varieties of Turmeric, which contain a large amount of a compound called Curcumin, Japanese White Turmeric is low on Curcumin and high on Labdane-type Diterpenes.
These Labdanes have been found to reduce and control inflammation, inhibit the growth of synovial membrane and slow Hyaluronic Acid loss, which means that there will be far less inflammation-related damages and more Hyaluronic Acid for synovial fluid creation and longer-lasting joints [26].
Two clinical trials in Japan were conducted, first with 60 participants in an in-house open study and second with 30 patients at Sodegaura Hospital. In both trials, all participants had significant improvements in their pain rating on the Visual Analogue Scale (VAS) after 4-8 weeks (1-2 months) of taking the supplement.
As there is a patent on the plant and its medicinal properties, only Turmeron Joint and its allied companies can sell it as a supplement. Japanese White Turmeric is only grown between March and November and only harvested once a year.
Once harvested, the plant is dried and the active ingredient extracted and turned into a capsule for your consumption. Everything is processed at a manufacturing facility with techniques that exceed GMP and FDA standards. Turmeron Joint took 17 years to develop.
Two Patents have been taken out on Japanese White Turmeric. The first on its extract and the second on the powder form of the dried root. Both patents were taken for their effectiveness in preventing arthritis by preventing the synovial membrane from growing abnormally [27] [28].
Further research is being done to ascertain the effectiveness of Japanese White Turmeric and its ingredients in treating osteoarthritis, including a Double-Blind Placebo-Controlled Randomized Clinical Trial with Labdanes. The experiment will be completed in July 2020 and the results will be released after the conclusion of this trial.
Find out more about Japanese White Turmeric here!
Dr Henry Chan is an orthopaedic surgeon practising at Mount Elizabeth Hospital. Dr Chan specializes in the management of adult and child fractures and trauma, general orthopaedic injuries, sports injuries of the ligament and meniscus, and degenerative spine conditions including prolapsed intervertebral discs (slipped discs). In his free time, he enjoys singing karaoke.

