In Singapore, about 1,900 people are diagnosed with colorectal cancer every year. It is the most common form of cancer in men above the age of 50.
Seeing blood in your stools can be frightening. However, it does not always mean that you have colorectal cancer. There are many other telltale signs.
In this guide, I will cover topics about colorectal cancer that you should know about. They include:
- types of treatment methods
- ways to diagnose it
- ways to reduce your risk of getting it
Read on to find out.
You can also read more about finding a Vascular Surgeon here.
What is colorectal cancer?
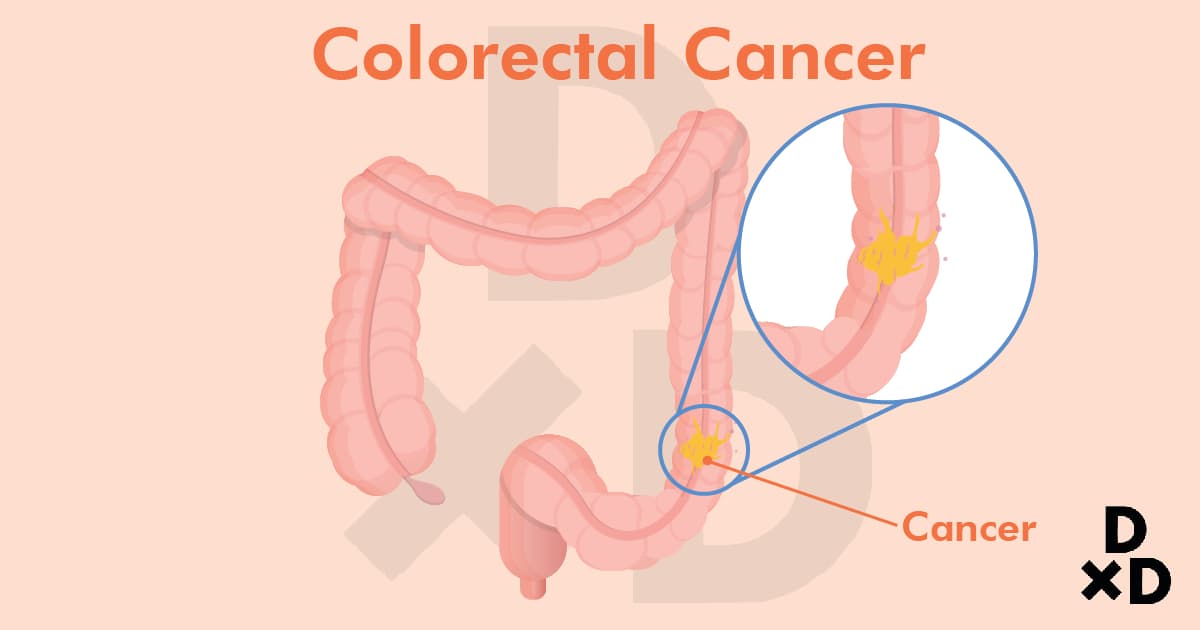
Colorectal cancer is a cancer that is found in the large intestine, or colon. The function of the colon is to:
- absorb water and electrolytes from waste products
- produce and absorb certain vitamins
- allow bacterial fermentation
- store faeces
- move faeces towards the anus
Colorectal cancer arises from the innermost layer of the 4-layered colonic wall. This is the layer that is in contact with stools and helps absorb nutrients from your stools [1].
How common is it?
Colorectal cancer is the most common cancer to affect Singaporeans. Among men, it is the:
- most common cancer for men above the age of 50
- 2nd-most common cancer for men below 50.
Meanwhile, for women, it is the:
- 2nd-most common cancer overall
- most common cancer post-menopause
While many of these patients can be cured, more than 50% are in the advanced stages of the cancer. Stage-3 and stage-4 cancers have a poor chance of cure.
The risk of developing colorectal cancer rises with age. Around the world, the risk rises gently from the age of 20 but dramatically after 50.
In Singapore today, about 20% of colorectal cancer patients are below 50. 20 years ago, the figure was below 10%. Evidently, there is a trend towards colorectal cancer occurring at younger ages.
How does colorectal cancer develop?
There are 4 layers in a normal colonic wall. The innermost layer is called the mucosa, where cancer cells can arise.
Before it can become cancerous, a normal colonic mucosal cell must undergo some changes. These changes happen in the genes of the cells, and are called genetic mutations.
It takes 10 to 15 years for a normal cell to transform entirely into a cancerous cell. While we know some of the defects, we do not fully know what triggers them.
Some of these abnormal genes can also be inherited. If one has an abnormal gene, the conversion process is faster.
The colonic mucosal cell grows larger as it changes, appearing as a lump called a polyp, and protrudes into the lumen of the colon. As defects develop, the polyp grows larger. Eventually, cancer develops within the polyp.
When the colorectal cancer gradually develops, it grows towards the outer layers of the colonic wall. It can then spread into the blood or lymphatic vessels. The lymphatic vessels drain into lymph nodes outside of the colonic wall. These lymph nodes help to trap cancer cells from spreading further.
However, if the cancer cells enter the blood vessels, they can travel far and wide to other internal organs. This process is known as metastasis.
What are the signs of colorectal cancer?
In the polyp, or precancerous, phase, there are usually no telltale signs. A colonic polyp is considered large when it is more than 1cm in length.
With that said, it may bleed as stools brush across its surface. This may be seen as small streaks of blood in the stools. Sometimes, the amount of blood is so little that it cannot be seen with our naked eyes.
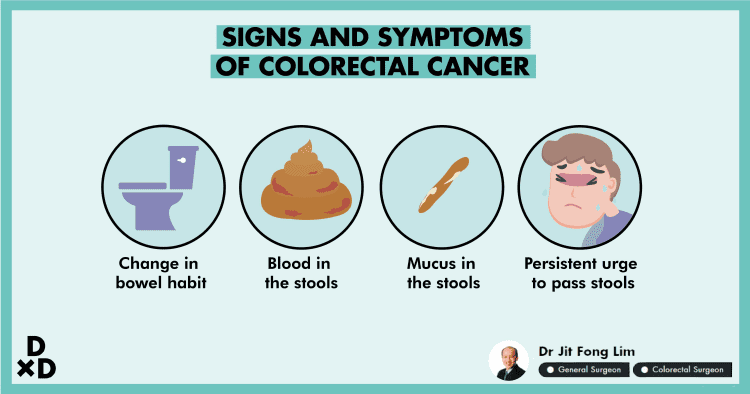
When one has developed colorectal cancer, the common symptoms are [2]:
- changes in bowel habits
- blood in the stools
- mucus in the stools
- a constant urge to pass stools
It might be a sign of colorectal cancer if:
- your bowel habits have changed
- this change persisted for more than 2 weeks
Changes in bowel habits
Everyone experiences changes in bowel habits from time to time. In normal cases, these will be resolved within 2 weeks.
If you develop cancer in the rectum, it can feel like a lump of stool is stuck inside your rectum. You will constantly feel like you need to pass stools but nothing comes out.
Some factors to look out for are:
- frequency of passing stools
- size of the stool
- colour of stools
In the more advanced stages of colorectal cancer, you may feel a lump in your abdomen (perhaps when you shower). Moreover, you may develop persistent abdominal bloating or suffer pain before passing stools.
Blood in stools
If you see blood in your stools or when you wipe yourself after passing stools, you should consult your doctor for further advice. Colorectal cancer is not the most common cause of blood in stools. With that said, it is the most important diagnosis that should be excluded.
Mucus in stools
If you pass mucus in your stools, it will appear like clear phlegm mixed with stools. Sometimes, you may think you have diarrhoea. However, the stool is not watery but is solid and mixed with mucus.
What happens when the cancer blocks your colon?
When that happens, you may develop abdominal distension, abdominal pain or vomiting.
In rare cases, the cancer can burst through (perforate) your colon. This causes sudden and severe abdominal pain.
Furthermore, if the cancer has been present for a long time or has spread to other organs of your body, you may become pale from anaemia (low red blood cell count). Anaemia happens because the cancer bleeds continuously. You may feel tired all the time.
In addition, the cancer can secrete proteins that make you lose your appetite. Thus, you may also lose weight.
If you know someone who looks pale or has lost a lot of weight without reason, you should encourage the person to seek medical attention soon.
Symptoms of possible colorectal cancer [3]:
- changes in bowel habit for more than 2 weeks
- blood in the stools
- mucus in the stools
- a frequent urge to pass stools
- unexplained anaemia (pallor)
- persistent weight loss
- loss of appetite
- abdominal bloating or pain
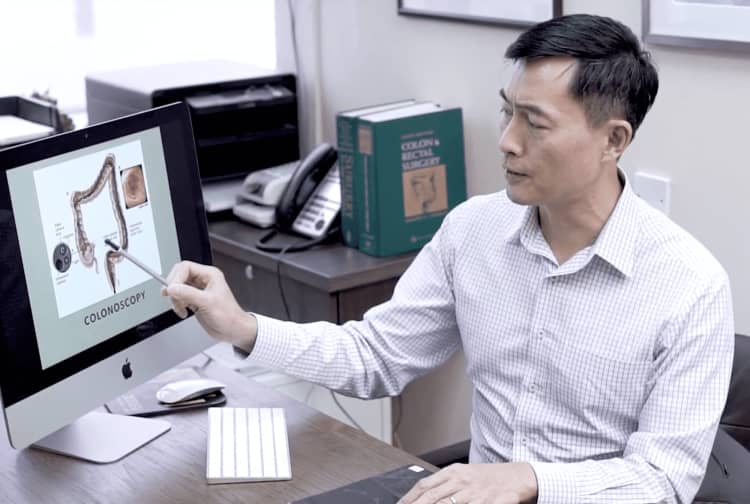
Ways to diagnose colorectal cancer
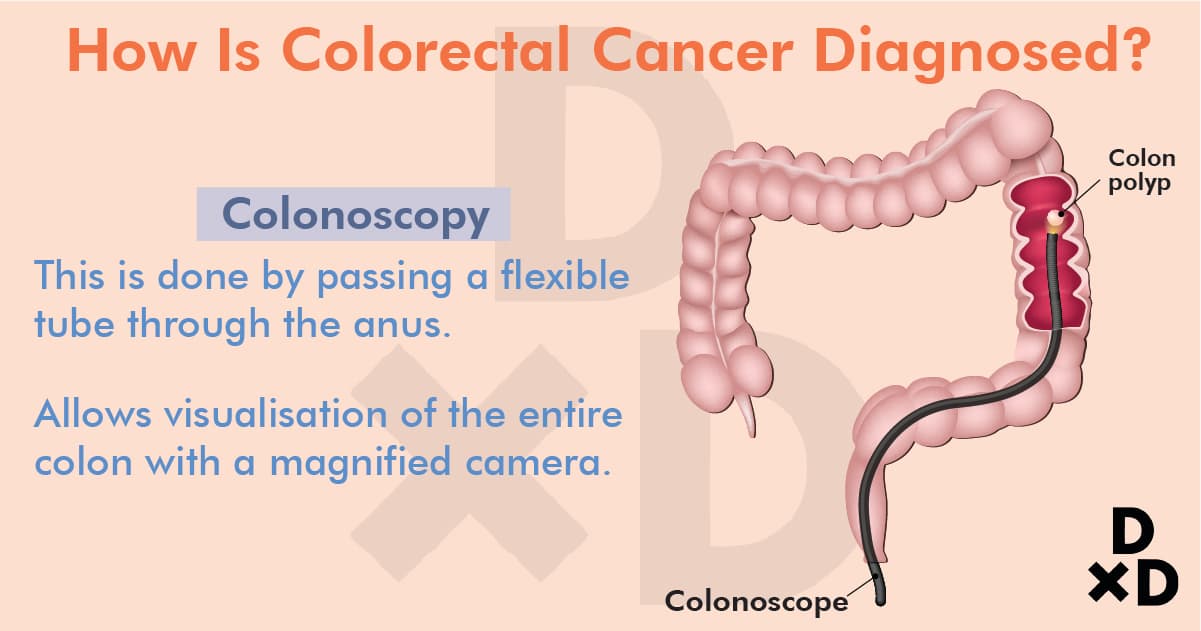
The most accurate test to confirm colorectal cancer is a colonoscopy. It works by passing a flexible tube through the anus to see the entire colon with a magnified camera. If polyps are present, these can be cut away (excised) and removed before they become cancerous. A tissue biopsy can be also taken to help plan treatment if cancer is present.
To assess the colon and abdomen, a computed tomography (CT) scan may be required. It is conducted in some cases where a colonoscopy cannot be performed. A CT scan is not as effective as a colonoscopy because polyps cannot be removed. Furthermore, a biopsy cannot be taken from the suspected cancer.
Patients will need to undergo blood tests and radiologic scans. This process starts after the confirmation of the cancer.
Scans such as a CT scan or magnetic resonance imaging (MRI) are used to plan treatment. Your doctor will advise you on the best options specific to your cancer. So be sure to consult a doctor to get your symptoms diagnosed.
How to treat colorectal cancer?
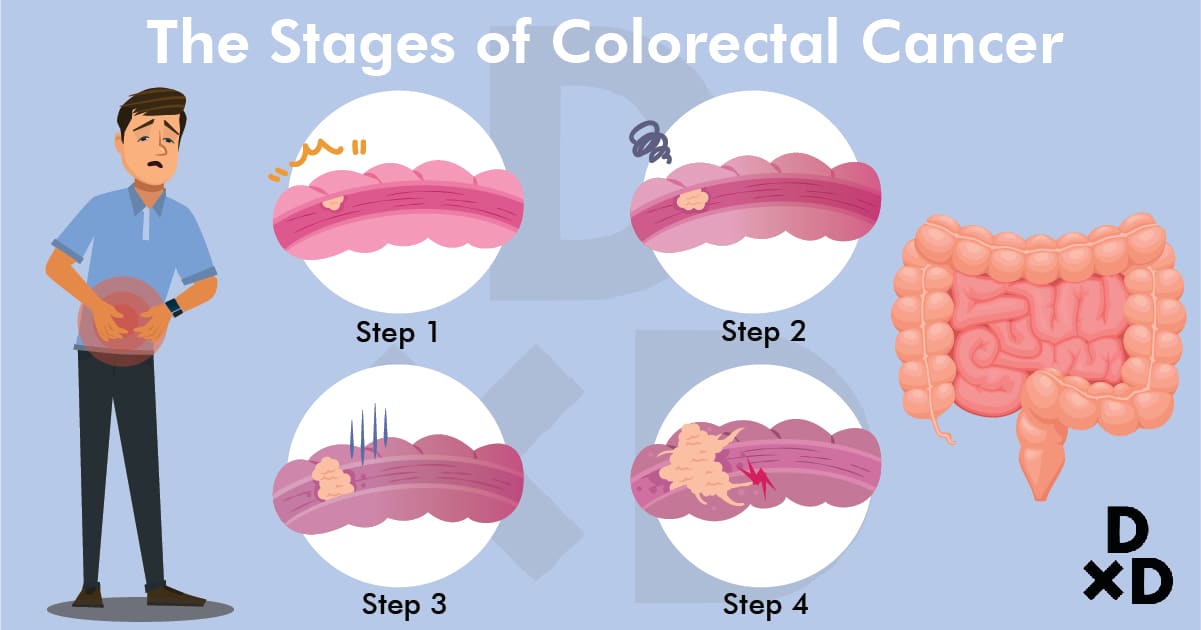
Treatment options for colorectal cancer are dependent on the stage of the disease. There are 4 stages of colorectal cancer.
Surgery
It is the cornerstone of treatment. You must consult a surgeon who specialises in colorectal surgery. A trained colorectal surgeon can perform the surgery in a precise manner.
Good-quality surgery can greatly improve the rate of recovery for patients with colorectal cancer. Most patients are also suitable for laparoscopic (keyhole) surgery, which shortens the recovery period and reduces complications.
For more than 95% of the patients who undergo surgery, a single-stage surgery is performed where:
- the segment with cancer is excised
- the two ends of the bowel joined back (anastomosed) immediately
Fewer than 5% of patients will need to wear a stoma bag. The majority of those with stomas can have the stoma reversed at a later surgery. Only about 1% to 2% of patients will need to wear a stoma bag permanently.
Stage
Description
Actions to be taken
1
The cancer is confined to the inner layers of the colon wall.
Surgery to remove segment containing cancer.
2
Cancer cells have reached the outer layer, but have yet to spread elsewhere.
Surgery is the only treatment unless there are unique features of your cancer that raises your risk of cancer recurrence. Chemotherapy may be required if there are high-risk features after surgery.
3
Cancer cells have spread to the lymph nodes. These lymph nodes are located outside the colon wall, adjacent to the blood vessels of the colon.
To maximise the rate of cure, a combination of chemotherapy, radiotherapy and surgery is often needed.
4
Cancer cells have spread to other internal organs.
Palliative treatments to ease symptoms.
In stage 4, while the prognosis is grim for many patients, some patients respond well to initial treatment.
To allow for a potential cure, cancer can be downstaged. However, downstaging is a complex topic and your cancer specialists will discuss this with you if needed.
Chemotherapy and Radiotherapy
There are times where I feel that patients may benefit from chemotherapy or radiotherapy. With that said, I will work with a medical and radiation oncologist specialising in colorectal cancer.
There have been significant improvements in medical and radiation oncology over the past 20 years. Many patients who undergo these treatments today have few side effects and complications are becoming rarer. The majority can also perform normal activities during treatment, with no visible effects.
Here are some common side effects:
- temporary numbness of the hands and feet during treatment
- temporary darkening of the skin
- abdominal bloating
Meanwhile, here are some of the more uncommon side effects:
- hair loss
- weight changes
- blood clotting problems
Lately, there are newly developed drugs that have attracted interest. They target cancer cells uniquely. These “targeted therapy” drugs are not indicated in the majority of colorectal cancer patients. However, there are rare cases where the genetic profile of the cancer shows that these drugs are suitable.
With that said, in these cases, the medical oncologist will discuss this option with the patient. Whenever in doubt, consult your doctor to find out which treatments are more effective for you.
Cure rate of colorectal cancer
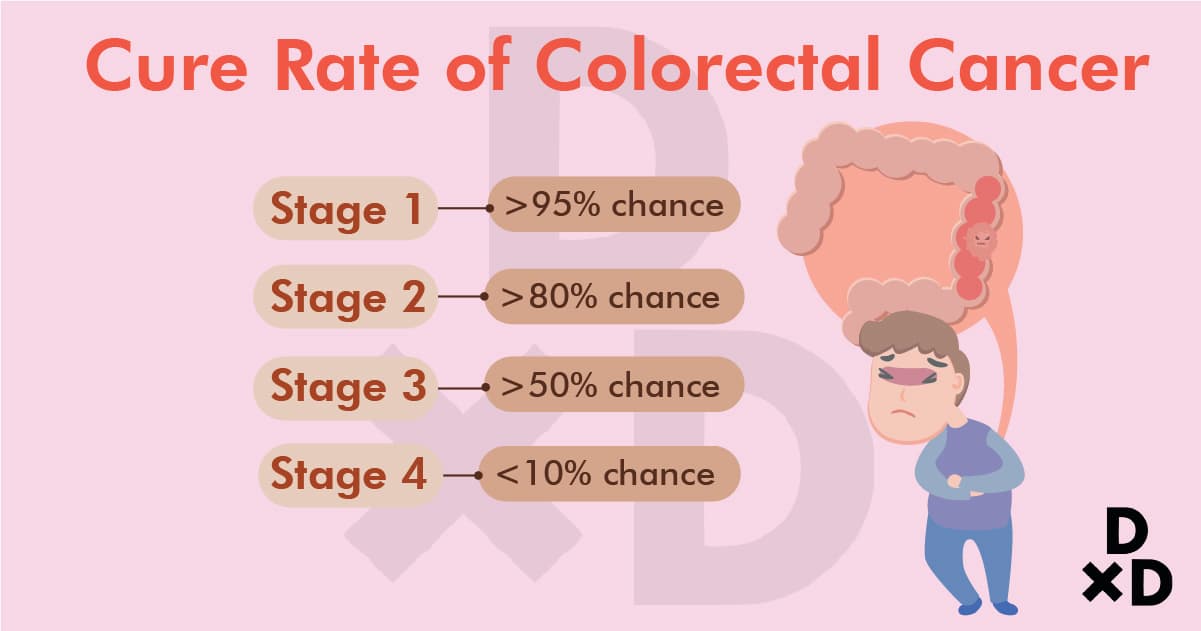
The overall cure rate for colorectal cancer is dependent on:
- the stage of the disease
- quality of surgery
- response to treatment
Stage
Chance of cure after surgery in most patients
1
more than 95%
2
more than 80%
3
more than 50%
4
less than 10% for those who respond well to treatment
Chance of downstaging cancer: more than 30%.
Thus, the main point here is that early diagnosis leads to the best chance of cure.
What if I do not get my colorectal cancer treated?

Colorectal cancer, if left untreated, will continue to grow.
The colon is essentially a tube to allow stools to pass to the anus. If the cancer encircles the circumference of the colon, it may obstruct the passage of stools. This is also known as intestinal obstruction.
When that happens, your abdomen will bloat and the blocked intestine will cause pain. When the blockage worsens, you may vomit.
The increasing swelling of the blockage can cause the colon to perforate. Perforation of the intestine without surgery will cause death within a week.
In some cases, the cancer does not cause intestinal obstruction or perforation but spreads to other internal organs. The cancer cells cause appetite loss and drain your energy. This leads to weight loss and the internal organs affected by cancer can deteriorate and fail. If internal organs like the liver or lungs fail, the outcome is catastrophic. If the cancer cells spread to your bones or nerves, it can cause persistent pain that can only be ameliorated by strong painkillers.
I want to let you know that in rare cases your doctor may advocate the option of not treating you aggressively. I will consider this option if:
the cancer has advanced, thus making it incurable, or
you suffer from significant medical conditions that increase your risk of death from treatment
(for example, an elderly patient with kidney failure requiring regular dialysis who also has stage 4 colorectal cancer)
Speak to your colorectal surgeon and talk about all your options. When you have doubts, you should seek a second opinion from another colorectal surgeon.
How can I reduce my risk of colorectal cancer?
Firstly, you need to understand the factors that affect the risk of colorectal cancer. This will allow you to know how to reduce the chances. There are risk factors you cannot change and those you can [4].
Unchangeable Factors
Factors you cannot change are:
- Age
- A family history of colorectal cancer or polyps
- IBD, or also known as Inflammatory Bowel Disease
- Inherited cancer syndromes
- Ethnicity
Age
While the risk of getting colorectal cancer increases with age, we are seeing more patients develop colorectal cancer before 50 years old. This pattern is similar around the world.
The risk continues to increase when you grow older, even after the age of 80 years.
Family history of colorectal cancer or polyps
About 1 out of 5 colorectal cancer patients have a family member who has had colorectal cancer or polyps before.
The risk of colorectal cancer increases if one of your first-degree relatives has cancer or polyps. If 2 of them have it, your risk is doubled! First-degree relatives include your:
- parents
- siblings
- children
Inflammatory bowel disease (IBD)
Patients suffering from IBD are at a higher risk. They will require regular colonoscopic surveillance. This even applies to those who have their disease well controlled.
Types of IBD include ulcerative colitis and Crohn’s disease.
Inherited cancer syndromes
A handful of people who develop colorectal cancer have inherited gene defects (mutations) that cause the disease. Often, these defects lead to cancer that may occur at a young age.
In Singapore, the percentage of colorectal cancer patients with inherited cancer syndromes is unclear.
About 5% of patients may have inherited cancer syndromes. Identifying families that have these inherited syndromes is important. Screenings and other preventive steps can be taken at a much earlier age.
Ethnicity
A person’s ethnicity affects his/her risk of colorectal cancer. In Singapore, the risk is the highest among Chinese, compared with Malays and Indians. Indians have the lowest risk out of the three races.
A similar pattern can be seen in America. African-Americans have a higher risk of colorectal cancer than Caucasians.
In short, all the factors mentioned in the past few sections cannot be changed. But identifying them helps you determine when you should be screened for possible colorectal cancer. Even if you do not have any symptoms yet, you should go for a screening.
Changeable Factors:
While there isn’t anything you can do about unchangeable factors, something can be done about these factors:
- Diet
- Smoking habits
- Alcohol consumption
- Obesity [5]
- Physical inactivity
Diet
A diet high in fibre can reduce your risk of colorectal cancer. Your diet should include:
- fruits
- vegetables
- whole grains
Conversely, a diet high in red meat and processed meat can increase your risk. Cooking food at high temperatures (such as grilling and barbecue) also raises the risk.
Smoking & Alcohol Consumption
Smoking increases your risk of colorectal cancer about twofold. The carcinogens from smoking are more well-known for their association with lung cancer, but they also increase the risk of many other types of cancers, including colorectal cancer.
Consuming more than 2 alcoholic drinks a day also increases the risk of colorectal cancer.
Obesity & Physical inactivity
Obesity is associated with an increased risk of colorectal cancer. It also has the potential to increase your risk of complications when you undergo treatment.
What is often under-reported is the potential benefits of an active lifestyle.
People who regularly engage in exercise at a moderate intensity have a 30% to 40% lower risk compared with people who do not. Examples of such exercises are jogging and swimming three times a week for at least 30 minutes.
Exercise induces the body to repair your muscles. This process also helps the body identify abnormal cells and repair them. Thereby, this reduces your risk of cancer.
Regular exercise also helps reduce the risk of:
- lung cancer
- prostate cancer
- breast cancer
Recommendations
Therefore, my recommendation to reduce your risk is to:
- exercise regularly
- stop smoking
- eat more vegetables and fruits
- reduce your red meat consumption [6]
These recommendations are very similar to the those that reduce the risk of hypertension and heart diseases.
How can I prevent or screen for colorectal cancer?
The dietary and lifestyle recommendations above can help you reduce the risk of colorectal cancer.
However, even if you adopt a healthy diet with good lifestyle habits, it does not mean that you are free from colorectal cancer. Ageing and inherited genes can also increase your risk of colorectal cancer. Therefore, you should consider colorectal cancer screening.
The Ministry of Health first published guidelines on screening for colorectal cancer in 2003. These guidelines were revised in 2019.
50 years old is the recommended starting age for all individuals to get screened [7]. When in doubt, always consult a doctor.
5 tests can screen for colorectal cancer. They are:
- Faecal occult blood test. Currently, Singapore uses the faecal immunochemical test, also known as FIT [8].
- Flexible sigmoidoscopy
- Flexible colonoscopy
- Barium enema
- CT colonography, also known as virtual colonoscopy
Related: The Ultimate Guide to Health Screening in Singapore (2021)
FIT
Today, the most widely performed test is the FIT. This test can be performed at home and it is the cheapest screening test available.
An instruction sheet can guide you on how to perform the test. The kit also contains a double-sealed bag coupled with a self-addressed envelope to send the sample to the hospital.
A colonoscopy will be recommended if the FIT shows blood in your stools. FIT is cost effective and can reduce the chance of death from colorectal cancer as it may diagnose cancer in its earlier stages.
However, FIT does not help prevent colorectal cancer [9].
Colonoscopy
A colonoscopy is the gold standard test to screen for colorectal cancer. It is the most accurate test and it allows your doctor to take a biopsy to confirm cancer.
More importantly, colonoscopy can detect pre-cancerous polyps. These polyps are usually silent, and don't come with any symptoms. Removal of the polyps prevents them from becoming cancerous.
A colonoscopy, along with the removal of pre-cancerous polyps, is the only method to date to prevent colorectal cancer.
Flexible sigmoidoscopy
A flexible sigmoidoscopy is like a colonoscopy. The main difference is that only the left half of the colon is assessed. It has been superseded by colonoscopy.
Barium enema
A barium enema is a radiologic test. It involves barium, a white liquid which can be seen on X-rays.
In the test, the barium is pumped into the rectum, followed by air. A series of X-rays are then taken to view the colon. During this process, you will be lying on a bed that can be tilted, which allows the barium to flow all the way through the colon.
This method is not well-liked by radiologists and patients alike. Therefore, it is used only if all else fails.
CT colonography
A CT colonography requires the patient to have a CT scan done in a prone and supine position. A computer software then merges the two scans to create a 3D image of your colon.
Due to the amount of radiation used, this test is also conducted only if colonoscopy fails.
Comparison
While all five tests are available, the FIT and colonoscopy are the tests that are regularly performed.
The table below summarises the screening guidelines for healthy individuals. They also should have no prior colorectal polyps or family history of colorectal cancer or polyps.
People with an increased risk of colorectal cancer will have a different set of guidelines. This is something that they should discuss with their doctor.
Screening Test
Age of onset for screening
Frequency
FIT
50 years old
Every year
Colonoscopy
50 years old
Every 10 years
Flexible sigmoidoscopy
50 years old
Every 5 years
Barium Enema
50 years old
Every 5 years
CT Colonography
50 years old
Every 5 years
In short
Colorectal cancer is the most common type of cancer to affect Singaporeans. It happens when colon cells transform into polyps and subsequently into cancerous cells.
The removal of precancerous polyps by colonoscopy can prevent colorectal cancer. This is the only known way to date to prevent this cancer.
A healthy diet and active lifestyle can help reduce your risk of developing colorectal cancer. Even with a good diet and lifestyle, everyone should go for colorectal cancer screenings when they reach the age of 50 years.
If anyone has signs and symptoms of this cancer, they should seek medical care promptly. When diagnosed in its early stages, colorectal cancer is highly curable.
You can beat the disease!
%treatmentquote title=Get quote for Colorectal Cancer%
Dr Lim Jit Fong is a colorectal surgeon at Lim Jit Fong Colorectal Centre. He specialises in general surgery as well as colorectal surgery. Dr Lim offers services ranging from the treatment of anal fissures to the treatment of functional disorders such as bowel incontinence. He also holds several appointments, one of which is president of the Society for Continence in Singapore.
Read more from Dr Lim Jit Fong in his Q&A here.