Human Session held on July 6, 2018.
Dr Gan Eng Cern is a fellowship trained Consultant Ear, Nose & Throat (ENT) Surgeon. He is well-versed in the management of a wide range of ENT conditions and has a passion for the treatment of conditions of the nose & sinuses as well as snoring and Obstructive Sleep Apnoea (OSA). He served as a Senior Clinical Lecturer at Yong Loo Lin School of Medicine at the National University of Singapore.
Dr Gan Eng Cern answered questions from readers on:
- Drippy noses
- Sinus problems
- Antibiotics for flu
- Cough and phlem that won't go away
How do I know if my breathing difficulties while running is due to a nose or heart problem?

Breathing difficulties during exercise can be dependant on several factors including:
1) Your age
2) Your fitness level
3) Your general health status. If you have a medical condition that may compromise the delivery of blood and oxygen to your vital organs, you can feel breathless on exertion or during exercise.
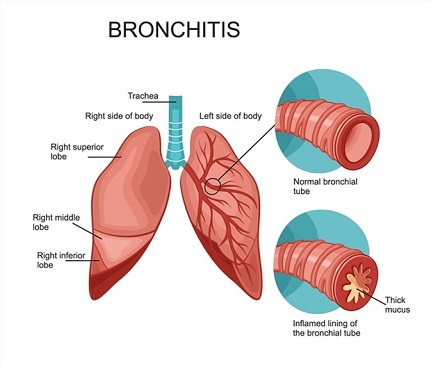
There can be many reasons for these including lung conditions (e.g Asthma, bronchitis), heart conditions (e.g. congenital defects), and conditions of the blood (e.g. low blood level).
4) Intensity of your exercise regimen
Blocked nose from a sensitive nose (Rhinitis) should not result in shortness of breath or difficulty in breathing. You may feel "more difficult to breathe" because you have to resort to mouth breathing when your nose is blocked, which may be uncomfortable. However, this shouldn't lead to inadequate oxygen flow to your lungs as your mouth and throat which is part of your upper airway should be able to cope with the increased airflow to your lungs during exercise.
If you have other symptoms such as chest pain, palpitation or light headedness during your run, you may have to see a Cardiologist who can perform stress tests to determine if your difficulty in breathing is due to a heart condition (less likely in a young patient like yourself unless there is an unknown congenital problem).
If after reading this you are still unsure, perhaps a visit to a General Practitioner will be a good start.
What is a permanent cure for sinus?

“Sinus” is a common term that many people incorrectly use to describe nose symptoms such as frequent blocked nose, runny nose and sneezing. Sinuses are hollow spaces that surround the nasal cavity. Everyone has them and it is a normal part of the anatomy in your face. The lining of these spaces (called mucous membranes) produces mucous that drains into the nose.
Sinusitis (infection of the sinuses, aka rhinosinusitis) occurs when the sinuses are blocked and trapped mucous in the sinuses are infected. Patients with sinusitis often present with nasal blockage, nasal congestion (feeling of mucous stuck in the nose or face – ie inability to blow the mucous out), facial pain (most often in the cheek, forehead and in between the eyes), postnasal drip and coloured phlegm or nose mucous.
The cure depends on the type of Rhinitis you have. If you have Allergic Rhinitis (tested positive for one or more allergens on a skin prick test), there is a potential cure known as Immunotherapy.
Immunotherapy involves desensitizing the patient to the known allergen by exposing them to small amounts of the allergen over a period of at least 3 years. The allergens can be given as an injection (called subcutaneous immunotherapy or SCID) or sprayed/placed under the tongue daily (called sublingual immunotherapy or SLIT).
Most ENT Clinics in Singapore use SLIT to treat patients with Allergic Rhinitis. This is the only known treatment that modifies the disease process and may offer a potential cure for Allergic Rhinitis.
How can I prevent frequent sinus infections?
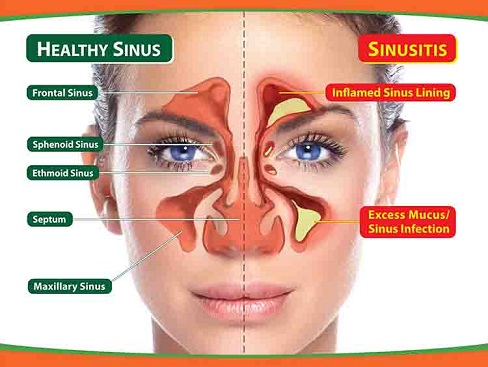
I am sorry to hear that you are experiencing sinus infections (medically known as sinusitis) every 1-2 months. It is important to determine if the "sinus infections" are indeed sinusitis. Common symptoms of a sinus infection includes:
- Blocked nose
- Facial congestion or pain
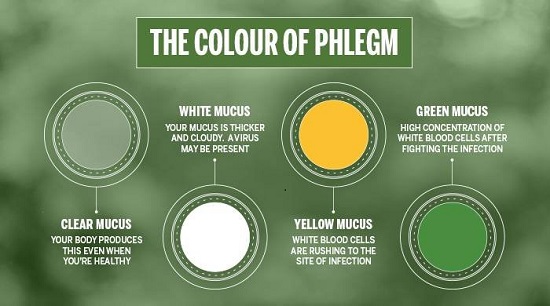
- Coloured nasal discharge/mucous (yellow, brown, green or even blood stained)
- Postnasal drip
- Reduced sense of smell
A sinus infection usually lasts longer than 10 days or continues to worsen on day 5 of your illness. If your symptoms are less than these, you may be experiencing a cold/flu (described medically as a viral upper respiratory tract infection or URTI).
It is important to differentiate between a cold/flu and sinus infection because one needs a course of oral antibiotics while the other doesn't. Sinus infections are caused by bacteria and a course of antibiotics will be required, while a cold/flu is caused by viruses and do not need to be treated with antibiotics.
There are certain risk factors that predisposes a person to getting more frequent sinus infections. These include nasal allergies (Allergic Rhinitis), deviated nasal septum, narrow sinus drainage pathways, smoking and genetic predisposition.
Prevention of frequent sinus infections depends on the underlying cause and sometimes a CT scan (special series of X-rays) of the sinuses may be required to assess any anatomical abnormalities that resulted in a blocked sinus or narrow sinus drainage pathway. If these are present, endoscopic sinus surgery to widen the drainage pathway of the sinuses while preserving its physiological function may be required.
Many of my patients with frequent sinus infections do have uncontrolled or poorly controlled nasal allergies. Keeping your nasal allergies under control may prevent frequent sinus infections.
When should I take antibiotics for a cold that’s not getting better?

As the common cold is usually caused by a virus, your body will fight it off within 7-10 days. You do not need antibiotics for this. Antibiotics does not work against viruses. You can take medications to relieve the symptoms of your cold, e.g. antihistamines and decontestants, lozenges, cough medications etc. These medications however do not help you fight off the cold. You are much more lightly to get better with adequate rest, sleep and good hydration.
If your symptoms are worsening on day 5 of your cold or the duration of your cold last longer than 10 days, it is likely that you have developed a bacterial sinus infection (known medically as sinusitis). These figures were derived from numerous studies to determine which group of patients will best benefit from a course of oral antibiotics if they suffer from a “prolonged cold”.
A bacterial infection of the sinus is treated with a course of oral antibiotics, nasal douche (wash of the nose with salt solution) and nasal steroid sprays. It is sometimes difficult to differentiate a cold from a sinus infection as the symptoms can be very similar. Having said that, a patient with a sinus infection tend to have less fever, body aches and sore throat and more facial pain.
What is the best treatment for post-nasal drip on one side of my nose?
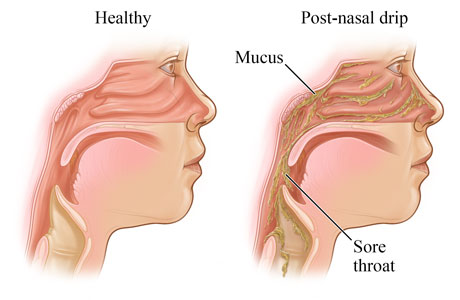
Common causes of postnasal drip (sensation of mucus stuck in the back of the nose or throat) include:
- Conditions of the nose (e.g sensitive nose or rhinitis, sinusitis)
- Acid reflux to the throat (called laryngopharyngeal reflux)
- Dehydration
In patients I’ve seen with similar history to yours, a one sided nasal congestion or postnasal drip may indicate an active sinus infection (sinusitis).
Since it has been ongoing for several months without relief from nasal steroid spray and antihistamine, and you’ve had previous sinus surgery (sphenoidoyomy), I would suggest consulting an ENT Specialist for evaluation.
Your ENT specialist will be able to perform a nasoendoscopy (scope through the nose) to examine the nasal cavity, sphenoid sinus and your voice box.
If you do have sinusitis, you will need a course of oral antibiotics and nasal douche (nose wash with salt solutions) in addition to the nasal steroid spray.
How do I get rid of a persistent cough?
Cough is a reflex that protects your upper airway from foreign materials and irritants. However, when persistent, it can be a troublesome symptom.
The cause of a chronic or prolonged cough can range from conditions arising from the nose (e.g. Rhinitis and Sinusitis), stomach (e.g. acid reflux from the stomach to the throat, medically known as Laryngopharyngeal reflux or LPR) and lungs (e.g. Asthma, Bronchitis etc) to side effects from medications (e.g. Blood pressure medications) and smoking.
If you have a wheeze associated with the cough and do get shortness of breath, you may have Asthma and should see a GP or Respiratory Physician. Your GP or Respiratory Physician may perform a lung function test to determine how much air moves in and out as you breathe.
In my practice, the two most common cause of chronic cough are due to a postnasal drip (which can be due to Rhinitis or Sinusitis) and Laryngopharyngeal reflux (LPR).
Are there any symptomatic treatments to help a persistent cough in an 8 year-old?

Common causes of chronic cough in children include problems arising from the nose and sinuses (e.g. allergic rhinitis, sinusitis), lungs (e.g. asthma, bronchitis, foreign bodies) or stomach (acid reflux).
The treatment of cough depends on the underlying cause. Since you mentioned that your daughter has been diagnosed with sensitive nose (Rhinitis), it is important to ensure that she has been compliant with her nasal steroid sprays for the treatment to be effective. Nasal steroid sprays work by reducing inflammation of the nose and sinuses and this can take up to 2 weeks before you notice significant improvement in nasal symptoms.
Although over the counter (OTC) cough medications (e.g. dextrometharphan, guaifenescin, antihistamines,codeine etc) may help ease cough in some children, a Cochrane meta-analysis (a summarized analysis of high level studies) has concluded that they are no more effective than placebo (medications with no cough suppresant properties) and may have potential side effects (e.g. drowsiness and insomnia).
In fact, 1-2 teaspoons of honey a day has been shown to be as or more effective than some OTC cough medications and with excellent safety profile (in children older than 2 years old).
Having said that, it is still more important to find out the reason for the cough and treat the underlying cause accordingly.
Is it possible to prevent the onset of croup and barking cough in paediatric patients?
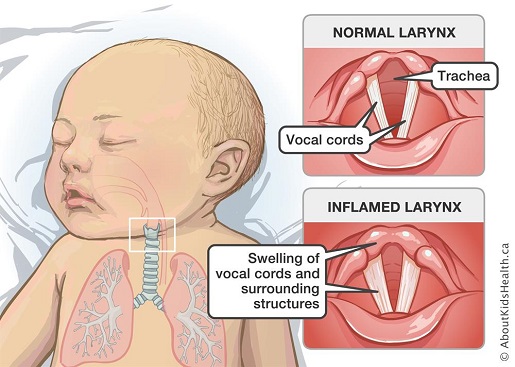
Croup is a viral infectious respiratory illness affecting mainly the voicebox, windpipe and sometimes the lungs. Many viruses can cause croup, including those responsible for the common cold and flu. Hence, the measure to prevent a croup are similar to that for a common cold.
These include practising good hand hygiene (by washing your hands regularly), coughing and sneezing into a tissue or into the elbow, cleaning surfaces regularly, avoiding food/drink sharing and keeping your children's immunization up to date.
In terms of medications, cough or cold medications have not been shown to be effective in the treatment of croup. Although the symptoms of a croup can be alarming, it is important to stay calm, sit your child upright and keep him/her well hydrated and well rested.
Most of the time, croup resolves on its own within 48 hours. Having said that, if your child has the following warning symptoms, he/she should visit the A&E:
- Struggling to breathe (heavy breathing sounds or you see his/her tummy sucked in during breathing)
- Skin looks blue
- Unusually quiet and still
Should I be concerned if my 4 year old has a dry cough and frequent nosebleeds?

Nosebleeds in children are most often due to prominent blood vessels on the front part of the nasal septum (wall that separates the nose into right and left sides) that have burst.
This can be spontaneous or triggered by certain activities such as frequent nose digging or violent sneezing. He may alsonbe suffering from Rhinitis (sensitive nose).
If the nosebleeds happen twice a week and he has troublesome sensitive nose, you should consider bringing him to see an ENT Specialist. If the cause of the nosebleed is due to enlarged blood vessels on the front part of the nasal septum, it can be easily sealed off using Silver nitrate sticks.
His sensitive nose can be treated with nasal steroid sprays and antihistamines.
What could be the cause of chronic cough at night and in early morning?
Since your mum has seen an ENT Specialist and was given an acid suppressant medication (Nexium) and nasal steroid sprays (to treat sensitive nose or nose allergies), it is important to ensure good compliance with these medications.
The importance of compliance with nasal steroid sprays is often overlooked by many patients. It can take days to weeks for nasal steroid sprays to reduce the mucous in the nose and postnasal drip (which may be a possible source of irritant of your mother’s cough).
Apart from taking Nexium, it is also just as important to ensure that your mother adheres to antireflux measures (e.g no food/drinks 3-4 hours before sleeping, taking small meals and avoiding reflux causing or “heaty” food).
If your mother has done all that I’ve mentioned above, it may also be worthwhile to get her doctor to examine the medications that she is taking (one of the common blood pressure medication can cause cough as a side effect).
Exposure to cigarette smoke can also persistently irritate the voicebox and prevent a full recovery. As your mother’s cough started after a chest infection, she may also have “Postinfectious Cough”, of which the reason is unfortunately unknown.
Some studies attribute this to excessive inflammation of the upper and lower airway after an infection, resulting in a persistent overproduction of mucous. This is difficult to treat and often needs mucous thinners/expectorants and cough medications to keep the symptoms under control or bearable.
If your mother’s cough is accompanied by a whooping inspiratory sound or leads to vomiting, she may need to revisit the Respiratory Physician to rule out infection that is due to B pertusis bacterial infection.
What should I do next if I still have green phlegm and cough after completing my course of antibiotics?
If you have a sinus infection and bronchitis that has not gone away with antibiotics, you can see an ENT Specialist for an assessment and likely a nasoendoscopy (scope through the nose done in the clinic under local anaesthesia).
If there is still infected mucous (mucopus) seen in your nose, a sample of the mucopus has to be taken and sent to the lab for analysis (bacterial culture). This is to determine the type of bacteria responsible for your sinus infection and the antibiotics that will be effective against that bacteria.
You should also be washing your nose with a nasal douche (salt water solution e.g. Neilmed or Flosinus) and apply nasal steroid sprays to your nasal cavities (e.g. Nasonex, Avamys or Nasacort). Most sinus infections do clear with a culture-directed antibiotics. If this fails, you may need a CT scan (speial series of X rays) of the sinuses to assess the severity of your blocked sinuses and the structural abnormalities that caused it.
If you have been refractory to medical treatments and have persistent sinus infection or structural abnormalities on the CT scan, you may need to undergo sinus surgery (functional endoscopic sinus surgery or FESS) to unblock the sinuses. This is a minimally invasive surgery done through the nose under general anaesthesia.
If you do not have a fever or shortness of breath, it is likely that your "bronchitis" is due to postnasal drip from the sinus infection causing accumulation of mucous in your throat region, resuling in phelgm and cough. If your ENT Specialist is concerned about a concurrent lung infection that failed to clear despite treatment of your sinusitis, he or she can refer you to a lung specialist.
Ever wanted to ask a health question to a specific renowned specialist in Singapore? Human Sessions are when these expert doctors answer all your questions!
View the complete list of upcoming Human Sessions here.







